Good health and well-being

Nine-month-old Sofia receives routine vaccinations and a medical check-up with her mother at a clinic in Bolivia.
© UNICEF/Radoslaw CzajkowskitoStagnating progress in reducing maternal mortality means a woman dies of preventable causes every two minutes
The global maternal mortality ratio (MMR) marginally declined from 227 deaths per 100,000 live births in 2015 to 223 in 2020. This figure remains over three times the target of 70 set for 2030 – meaning that approximately 800 women died every day from preventable causes related to pregnancy and childbirth, or one death every two minutes. From 2016–2020, the global average annual reduction rate was approximately zero, significantly lower than the 2.7 per cent rate achieved between 2000 and 2015.
In 2020, about 70 per cent maternal deaths occured in sub-Saharan Africa, followed by Central and Southern Asia at nearly 17 per cent. Fifteen-year-old girls in sub-Saharan Africa had the highest lifetime risk (1 in 40) – approximately 400 times higher than their peers in Australia and New Zealand. Between 2016 and 2020, LDCs and LLDCs saw significant drops in MMR, with an average annual reduction rate of 2.8 per cent and 3.0 per cent, respectively, while in SIDS, the annual reduction rate was only 1.2 per cent.
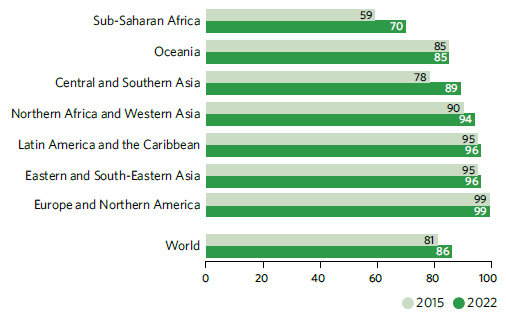
Global coverage of assisted childbirth by skilled health personnel has risen from 81 to 86 per cent between 2015 and 2022, but access remains limited in many countries, particularly in sub-Saharan Africa and Southern Asia, where mortality rates are highest. However, sub-Saharan Africa experienced the fastest growth, from 59 to 70 per cent between 2015 and 2022.
Proportion of births attended by skilled health personnel, 2015 and 2022 (percentage)
Progress on reproductive health continues, with falling adolescent birth rates and rising access to contraception
More women and girls now have improved access to sexual and reproductive health services. The proportion of women of reproductive age (15–49 years) having their need for family planning satisfied with modern methods has increased slightly, from 76.5 to 77.6 per cent between 2015 and 2023, and is projected to reach 78.2 per cent by 2030. Sub-Saharan Africa has witnessed the largest increase, from 51.6 to 57.4 per cent during this period, and is expected to rise to 62.1 per cent by 2030.
The global adolescent birth rate for girls aged 15–19 was 41.3 births per 1,000 girls in 2023, down from 47.2 in 2015. The global adolescent birth rate for girls aged 10–14, reported for the first time in the global monitoring of the Goals, has also declined from 1.8 births per 1,000 girls in 2015 to 1.5 in 2023. Latin America and the Caribbean reported the largest reduction, from 67.3 births per 1,000 girls aged 15–19 in 2015 to 51.4 in 2023, and from 3.3 births per 1,000 girls aged 10–14 in 2015 to 2.3 in 2023.
Global child mortality rates show significant decline, but challenges remain
A significant reduction in child mortality has been achieved over the past two decades. Between 2015 and 2021, the global under-5 mortality rate fell by 12 per cent, from 43 deaths per 1,000 live births to 38. Additionally, the global neonatal mortality rate fell by about 10 per cent, from 20 deaths per 1,000 live births to 18. Despite this progress, 5 million children still lost their lives before their fifth birthday in 2021, down from 6.1 million in 2015. Nearly half of those deaths (2.3 million) occured in the first 28 days of life. While child mortality has declined in all regions, sub-Saharan Africa continues to face the highest rates. In 2021, 1 child in 14 died before reaching age 5 (74 deaths per 1,000 live births) in this region, the same as the global average rate achieved two decades ago in 2001.
By 2021, 133 countries had already met the SDG target on under-5 mortality, and an additional 13 are expected to do so by 2030, if current trends continue. But to achieve the target by 2030, progress needs to accelerate in 54 countries, nearly 75 per cent of which are in sub-Saharan Africa. If these countries were to achieve the under-5 target, nearly 10 million under-5 deaths could be averted between 2022 and 2030. Meanwhile, more than 60 countries need to accelerate progress to meet the neonatal target.
Under-5 and neonatal mortality rate, 2015–2021 (deaths per 1,000 live births)
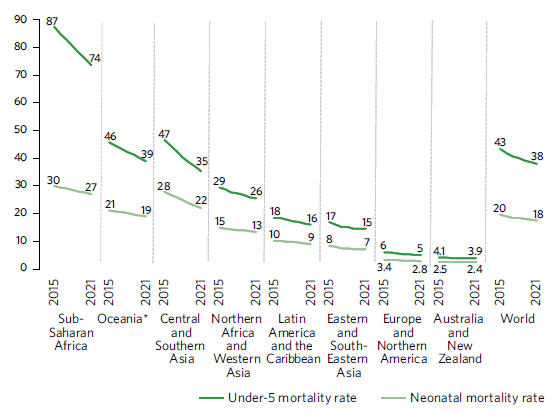
*Excluding Australia and New Zealand.
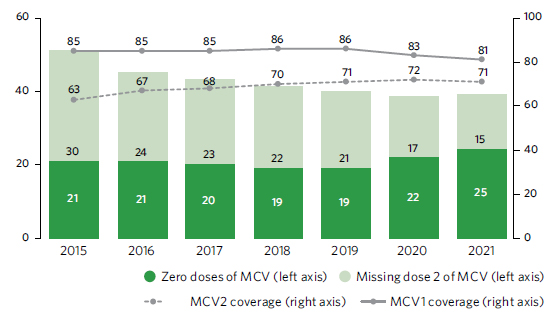
The alarming decline in childhood vaccination is leaving millions of children at risk from devastating but preventable diseases
The share of children who received three doses of the vaccine against diphtheria, tetanus and pertussis (DTP3) – a marker for immunization coverage within and across countries – fell 5 percentage points between 2019 and 2021, to just 81 per cent. This marked the largest sustained decline in childhood vaccinations in approximately 30 years. As a result, 25 million children missed out on one or more doses of DTP through routine immunization services in 2021 alone. This is 2 million more than those who missed out in 2020 and 6 million more than in 2019, highlighting the growing number of children at risk from devastating but preventable diseases. In 2021, only 70 per cent of children received two doses of the vaccine for measles, a highly contagious disease. This was far below the 95 per cent population coverage required to prevent outbreaks. Coverage of the first dose of human papillomavirus (HPV) vaccine, which has grave consequences for women and girls’ health worldwide, reached only 15 per cent in 2021, despite the first vaccines being licensed over 15 years ago.
Measles-containing vaccination (MCV) coverage, 2015–2021 (percentage) and estimated number of children missing doses of MCV, 2015–2021 (millions)
Intersecting crises have left the world off-kilter to achieve SDG targets on HIV, malaria and tuberculosis
HIV/AIDS: There were an estimated 1.5 million new human immunodeficiency virus (HIV) infections globally in 2021, almost one third fewer than in 2010. Effective HIV treatment has also cut global AIDS-related deaths by 52 per cent, from 1.4 million in 2010 to 650,000 in 2021. Sub-Saharan Africa, the region with the largest HIV burden, has achieved a 44 per cent decline in annual new HIV infections since 2010. However, the decline has been much sharper among males than among females. Fewer children were accessing treatment than adults. The aforementioned inequalities and others faced by key populations at increased risk of HIV are slowing progress towards ending AIDS. Moreover, new infections are rising in some regions, and the world is off track to meet the targets of fewer than 370,000 new HIV infections by 2025.
HIV incidence rates, 2010 and 2021 (new cases per 1,000 uninfected adults aged 15–49 years)
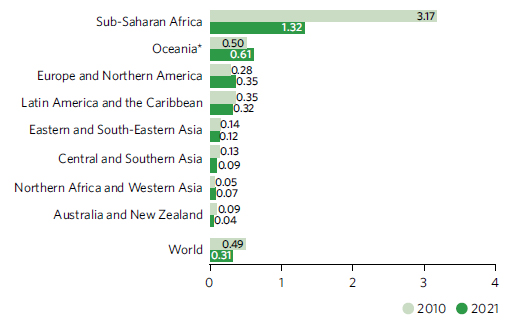
*Excluding Australia and New Zealand.
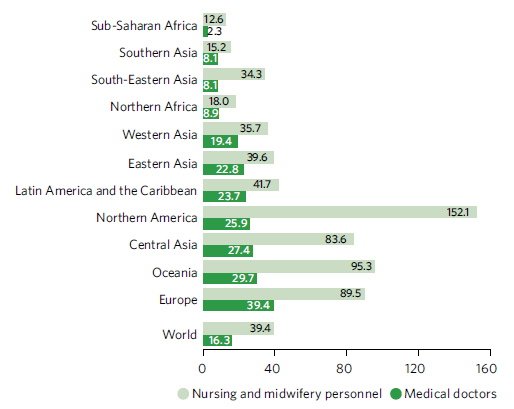
Tuberculosis (TB): The COVID-19 pandemic has severely impacted access to tuberculosis diagnosis and treatment in many countries, resulting in an increase in the TB disease burden globally. In 2021, an estimated 10.6 million people fell ill with TB, an increase from 10.1 million in 2020. The TB incidence rate also rose by 3.6 per cent between 2020 and 2021, reversing the decline of 2 per cent per year observed for most of the previous two decades. There were an estimated 1.6 million deaths from TB in 2021, an increase of 14.1 per cent from 2020. This is the first time in nearly two decades that the number of TB deaths has increased. Between 2015 and 2021, the net reductions in TB incidence and death were 10 per cent and 5.9 per cent, respectively, only one-fifth and one-tenth of the way to the 2025 milestone of WHO’s End TB Strategy.
Incidence rate of tuberculosis, 2015–2021 (new cases per 100,000 population)
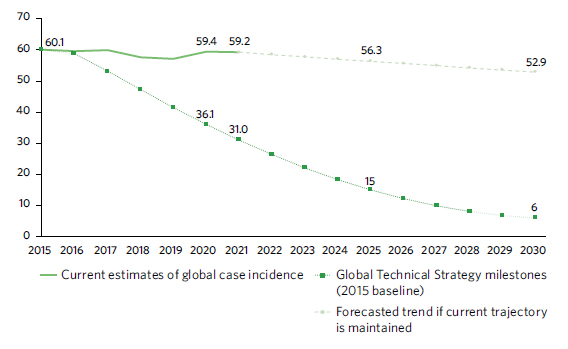
Malaria: In 2021, the global malaria death toll was estimated at 619,000, compared with 625,000 in 2020 and 568,000 in 2019. The total number of malaria cases worldwide reached 247 million in 2021, surpassing the figures of 245 million in 2020 and 232 million in 2019. Despite COVID-related disruptions, malaria-affected countries around the world largely maintained prevention, diagnosis and treatment measures at levels comparable to pre-pandemic times. In 2021, 128 million insecticide-treated nets reached their target destination, along with 223 million malaria rapid diagnostic tests and 242 million courses of artemisinin-based combination therapy. However, too many people at high risk of malaria are still missing out on the services they need to prevent, detect and treat the disease, and progress towards the ending malaria target by 2030 remains off course. In addition to pandemic-related disruptions, converging humanitarian crises, funding constraints, weak surveillance systems and declines in the effectiveness of core malaria-fighting tools threaten to undermine the global malaria response, particularly in Africa.
Two scenarios of global progress in the malaria incidence rate: current trajectory maintained and WHO Global Technical Strategy targets achieved, 2015–2030 (new cases per 100,000 population)
Neglected tropical diseases (NTDs): In 2021, 1.65 billion people were reported to require mass or individual treatment and care for neglected tropical diseases, down from 2.19 billion in 2010, representing a reduction of 25 per cent. As of December 2022, 47 countries, territories and areas have eliminated at least one NTD. In the LDCs, 46 per cent of the population required treatment and care for NTDs in 2021, down from 79 per cent in 2010.
In the wake of the pandemic, progress towards universal health coverage has slowed while financial hardship has risen
Universal health coverage (UHC) aims to ensure that everyone can access quality health services without facing financial hardship. While efforts to combat infectious diseases like HIV, TB and malaria led to significant expansions in service coverage between 2000 and 2015, progress has since slowed. The UHC Service Coverage Index only increased by three points since 2015, reaching a score of 68 in 2021. Meanwhile, components of UHC related to non-communicable diseases, health service capacity and access have seen minimal or no progress.
Financial hardship remains a significant challenge. The proportion of the population spending over 10 per cent of their household budget on health, out of pocket, worsened from 12.6 per cent in 2015 to 13.5 per cent in 2019, affecting around 1 billion people. Additionally, 4.9 per cent of the global population (around 381 million people) were pushed or further pushed into extreme poverty due to out-of-pocket payments for health in 2019.
Available evidence suggests a pandemic-related deterioration in UHC, with subregional and country-level decreases in the Service Coverage Index and disruptions in the delivery of essential health services. COVID-19 has also led to higher rates of foregone care and increased financial hardship due to high and impoverishing out-of-pocket spending. Accelerating the expansion of essential health services, particularly in areas with minimal progress, is crucial for advancing UHC. Proactive policies are needed to reduce financial hardship, increase public health funding, extend coverage for medicines and remove co-payments for the poor.
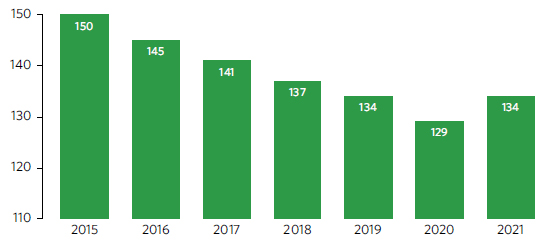
Despite increases in the global health workforce, numbers remain low in regions with the highest burden of disease
A 2020 study shows that the projected global shortage of health workers by 2030 has been reduced from 18 million to 10 million. Despite a significant increase in the overall size of the global health workforce, regions with the highest disease burden continue to have the lowest proportion of health workers to deliver health services. Between 2014 and 2021, sub-Saharan Africa continues to have the lowest health worker density, with only 2.3 medical doctors and 12.6 nursing and midwifery personnel per 10,000 population. In contrast, Europe had the highest density for doctors, at 39.4 per 10,000 population, while Northern America had the most nursing and midwifery personnel, with 152.1 per 10,000 population. Even when national densities seem adequate, disparities persist between rural, remote, subnational and hard-to-reach areas compared with capital cities and urban centres.
Density of select health professionals, 2014–2021 (per 10,000 population)
Driven by COVID-19, official development assistance for basic health has doubled since 2015
Official development assistant (ODA) for basic health from all donors has doubled in real terms since 2015, from $10.2 billion (constant 2021 prices) to $20.4 billion in 2021. Approximately $2.7 billion was spent on basic health care, $2.4 billion on malaria control, and $2.0 billion on infectious disease control. Germany, the United States, the Global Fund and Gavi, the Vaccine Alliance, accounted for almost 40 per cent of this total. In 2021, COVID-19 control represented the largest share of ODA for basic health, totaling $9.6 billion, of which $6.3 billion was for vaccine donations. Preliminary data for 2022 indicate that within total ODA, $11.2 billion was spent on COVID-19-related activities,1 down 45 per cent from 2021. Vaccine donations amounted to $1.53 billion, a fall of 74 per cent in real terms compared to 2021.
1 The figures in 2022 on COVID-19-related activities are preliminary and partial, as several donors are still in the process of collecting detailed information, especially sector-related data.

